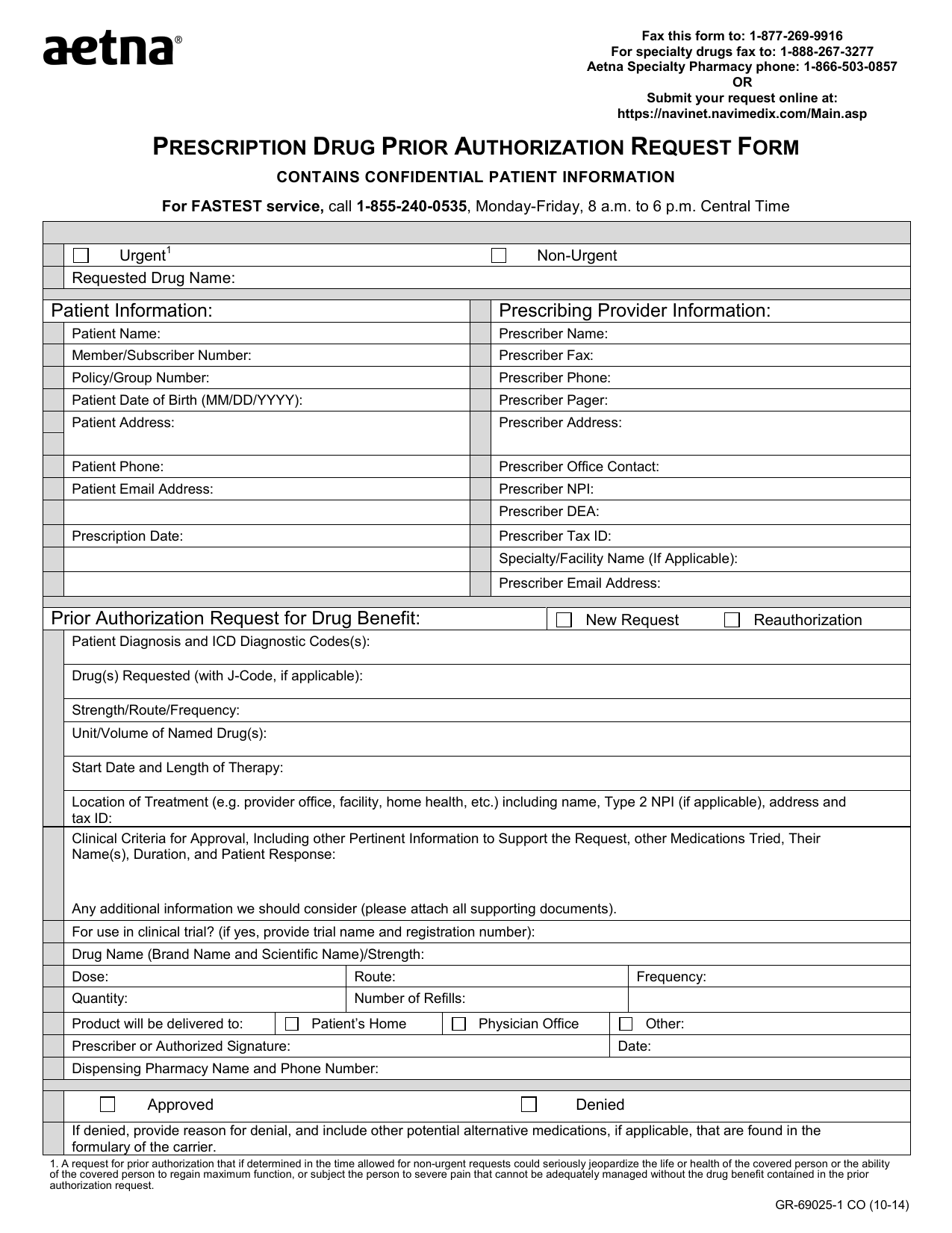
Aetna Prior Authorization Form For Specialty Medication
Aetna Prior Authorization Form For Specialty Medication - This is called prior authorization. Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Some care will require your doctor to get our approval first. You might also hear it called “preapproval” or. Web select the appropriate aetna form to get started. We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as: Covermymeds is aetna prior authorization forms’s preferred method for receiving epa requests. Procedures and services on the aetna. Web precertification occurs before inpatient admissions and select ambulatory procedures and services.
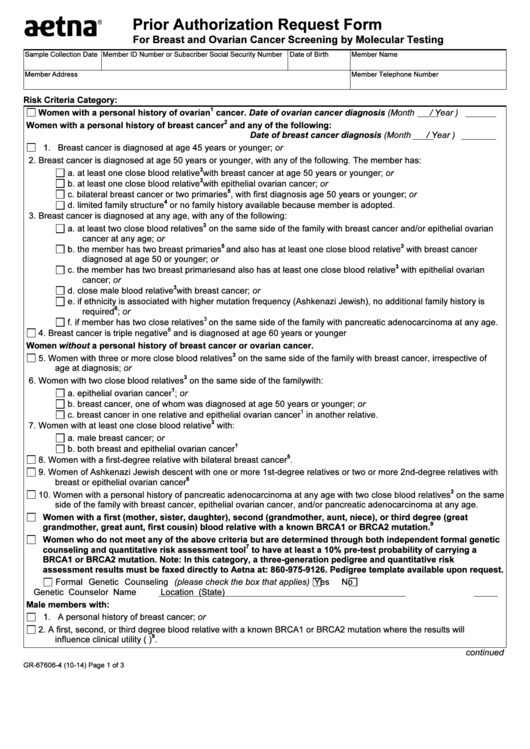
Web request prior authorizations on availity®. Medical specialty drug prior authorization. This process is called prior authorization or preapproval. Submit your request online at: Product information request is for: Web page 1 of 2 (you must complete both pages.) fax completed form to: Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery. Web what is prior authorization? Covermymeds is aetna prior authorization forms’s preferred method for receiving epa requests. You may now request prior authorization of.
Web page 1 of 2 (you must complete both pages.) fax completed form to: This is called prior authorization. It means that aetna better. Web aetna provides certain management services to these entities. Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery. Submit your request online at: Web health insurance plans | aetna Web what is prior authorization? Product information request is for: We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as:
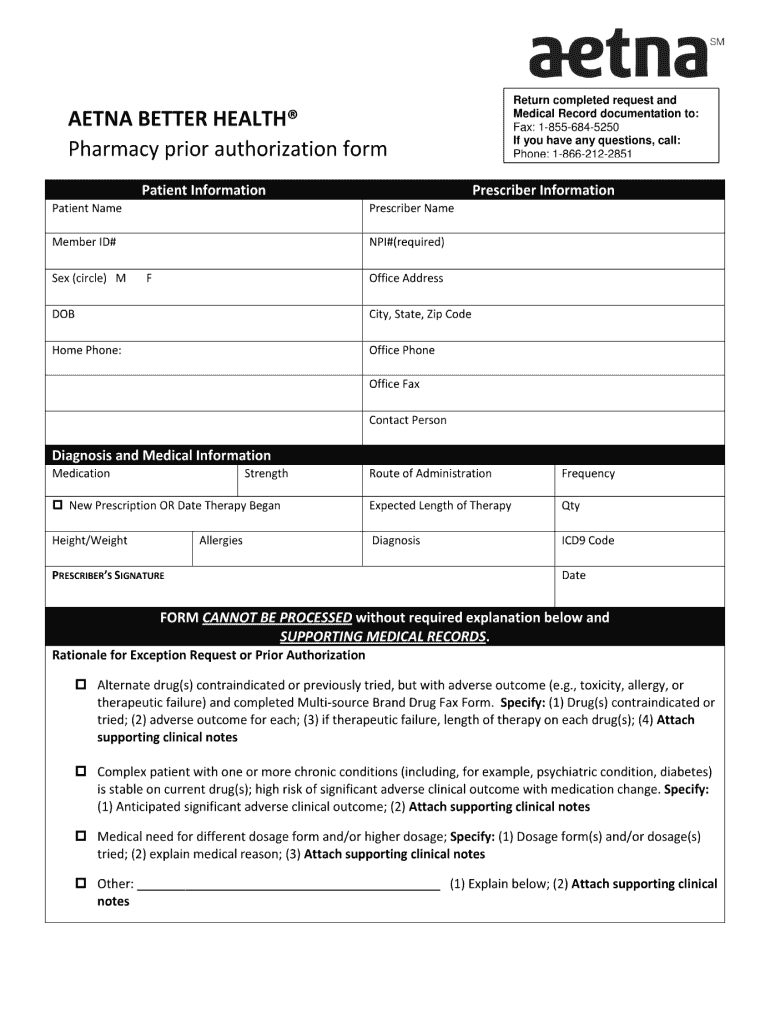
Aetna Prior Authorization Form Medical Record Health Sciences
Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web precertification occurs before inpatient admissions and select ambulatory procedures and services. Procedures and services on the aetna. Web in these cases, your doctor can submit a request on your behalf to get that approval. It means that aetna better.
xray request form fill online printable fillable blank pdffiller x
This process is called prior authorization or preapproval. Web what is prior authorization? Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery. We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as: Web select the appropriate aetna form to get started.
Aetna GR68285 Form 2011 Fill and Sign Printable Template Online US
Peer to peer consultations peer to peers are scheduled by calling 1. We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as: Web aetna provides certain management services to these entities. This process is called prior authorization or preapproval. Covermymeds is aetna prior authorization forms’s preferred method for receiving epa requests.
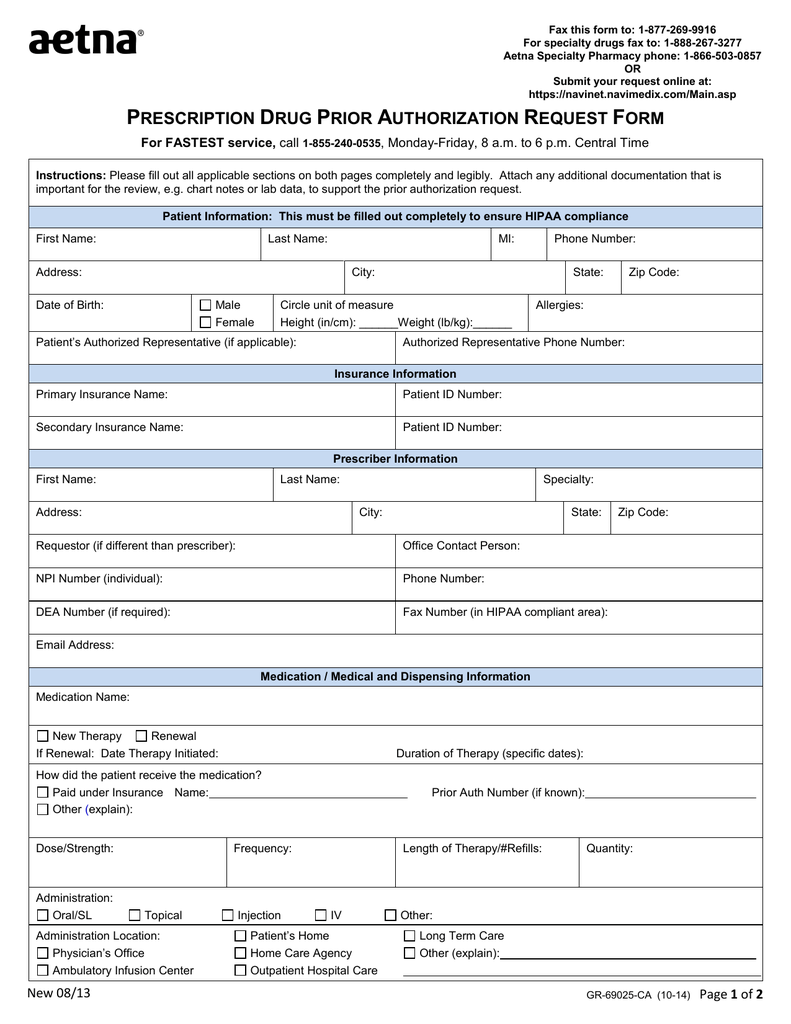
Download AETNA Prescription Drug Authorization Request Form PDF RTF
Web what is prior authorization? You might also hear it called “preapproval” or. Covermymeds is aetna prior authorization forms’s preferred method for receiving epa requests. Web fax this form to: We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as:
Aetna blank prior authorization forms Fill out & sign online DocHub
It means that aetna better. Peer to peer consultations peer to peers are scheduled by calling 1. Web aetna provides certain management services to these entities. Covermymeds is aetna prior authorization forms’s preferred method for receiving epa requests. Web select the appropriate aetna form to get started.
Prior Authorization Form For Medicare Advantage Universal Network
Web aetna provides certain management services to these entities. You may now request prior authorization of. Product information request is for: Web page 1 of 2 (you must complete both pages.) fax completed form to: Web request prior authorizations on availity®.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web fax this form to: Web health insurance plans | aetna Some care will require your doctor to get our approval first. This is called prior authorization.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Some care will require your doctor to get our approval first. Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery. Web what is prior authorization? We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as: Medical specialty drug prior authorization.
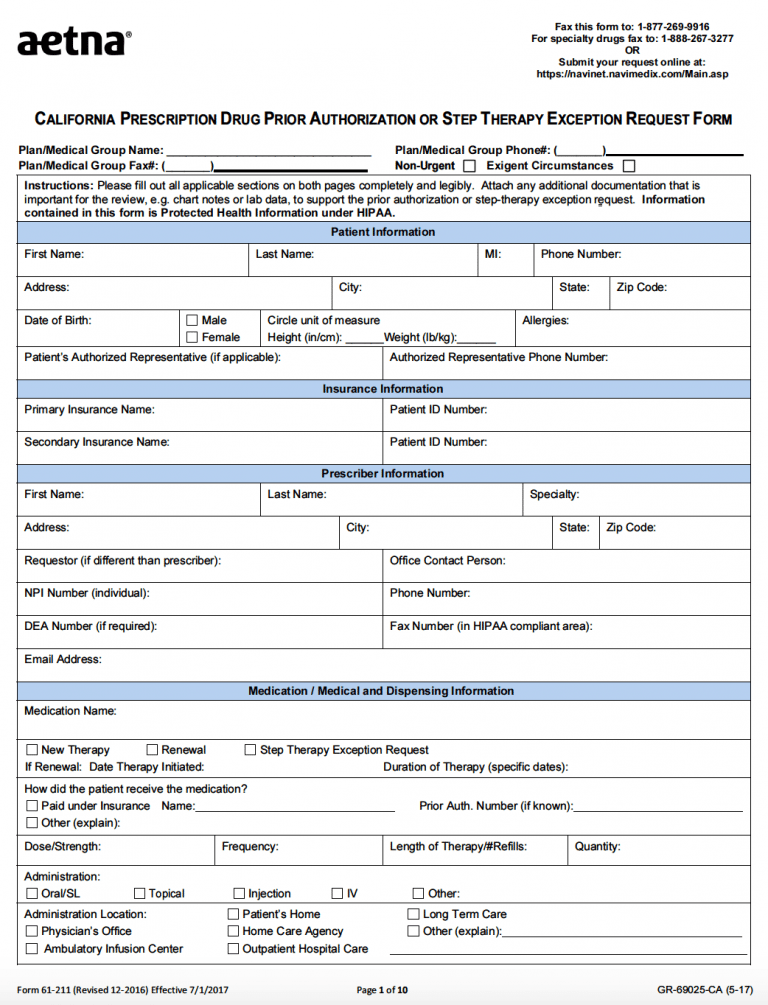
Free AETNA Prior Prescription (Rx) Authorization Form PDF
Web select the appropriate aetna form to get started. Submit your request online at: It means that aetna better. Product information request is for: Pharmacy specialty drug prior authorization.
Top 6 Aetna Prior Authorization Form Templates free to download in PDF
Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery. Pharmacy specialty drug prior authorization. Web in these cases, your doctor can submit a request on your behalf to get that approval. This process is called prior authorization or preapproval. Product information request is for:
Pharmacy Specialty Drug Prior Authorization.
Web health insurance plans | aetna Web what is prior authorization? Product information request is for: We’re making it easier to request authorizations and submit requested clinical information for selected procedures, such as:
Some Care Will Require Your Doctor To Get Our Approval First.
Web request prior authorizations on availity®. You may now request prior authorization of. Submit your request online at: Web medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application requests oral maxillofacial surgery.
You Might Also Hear It Called “Preapproval” Or.
Web aetna provides certain management services to these entities. Peer to peer consultations peer to peers are scheduled by calling 1. Web select the appropriate aetna form to get started. Covermymeds is aetna prior authorization forms’s preferred method for receiving epa requests.
Medical Specialty Drug Prior Authorization.
Web page 1 of 2 (you must complete both pages.) fax completed form to: It means that aetna better. This process is called prior authorization or preapproval. Web precertification occurs before inpatient admissions and select ambulatory procedures and services.