Aetna Prior Authorization Form Medication
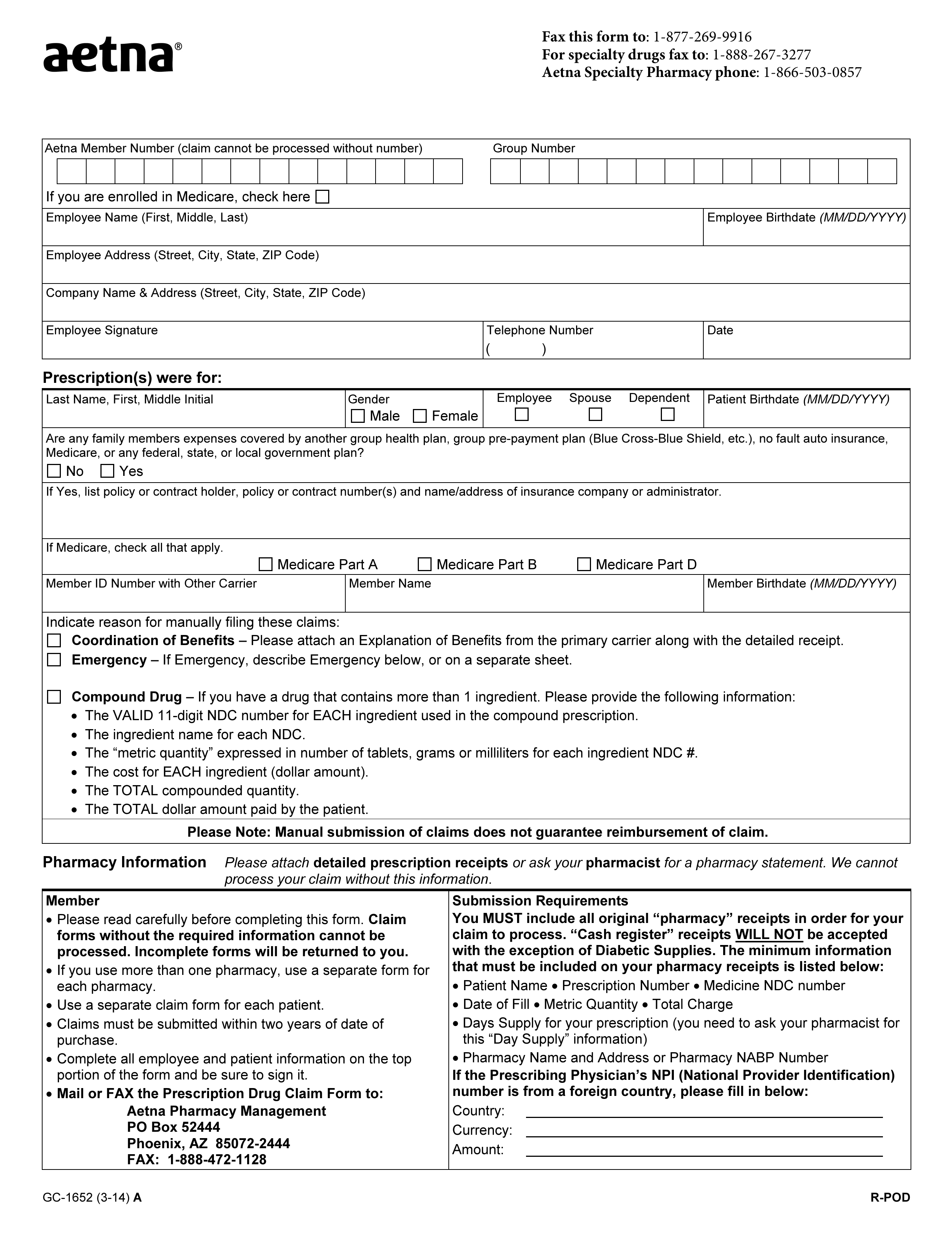
Aetna Prior Authorization Form Medication - Web prior authorization/precertification* request for prescription medications fax this form to: In these cases, your doctor can submit a request on your behalf to get that approval. You might also hear it called “preapproval” or “precertification”. Web what is prior authorization? Pharmacy specialty drug prior authorization. This is called prior authorization. Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment: Medical specialty drug prior authorization. Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as stated in the.
In these cases, your doctor can submit a request on your behalf to get that approval. Within the timeframe outlined in the denial notification. Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment: Web prior authorization/precertification* request for prescription medications fax this form to: You might also hear it called “preapproval” or “precertification”. Web submit your request online at: Medical specialty drug prior authorization. Start date / / aetna precertification notification continuation of therapy: Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Please attach supporting information, as necessary, for your request.
Within the timeframe outlined in the denial notification. Pharmacy specialty drug prior authorization. Web submit your request online at: In these cases, your doctor can submit a request on your behalf to get that approval. Please attach supporting information, as necessary, for your request. Some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web prior authorization/precertification* request for prescription medications fax this form to: Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment: You might also hear it called “preapproval” or “precertification”.
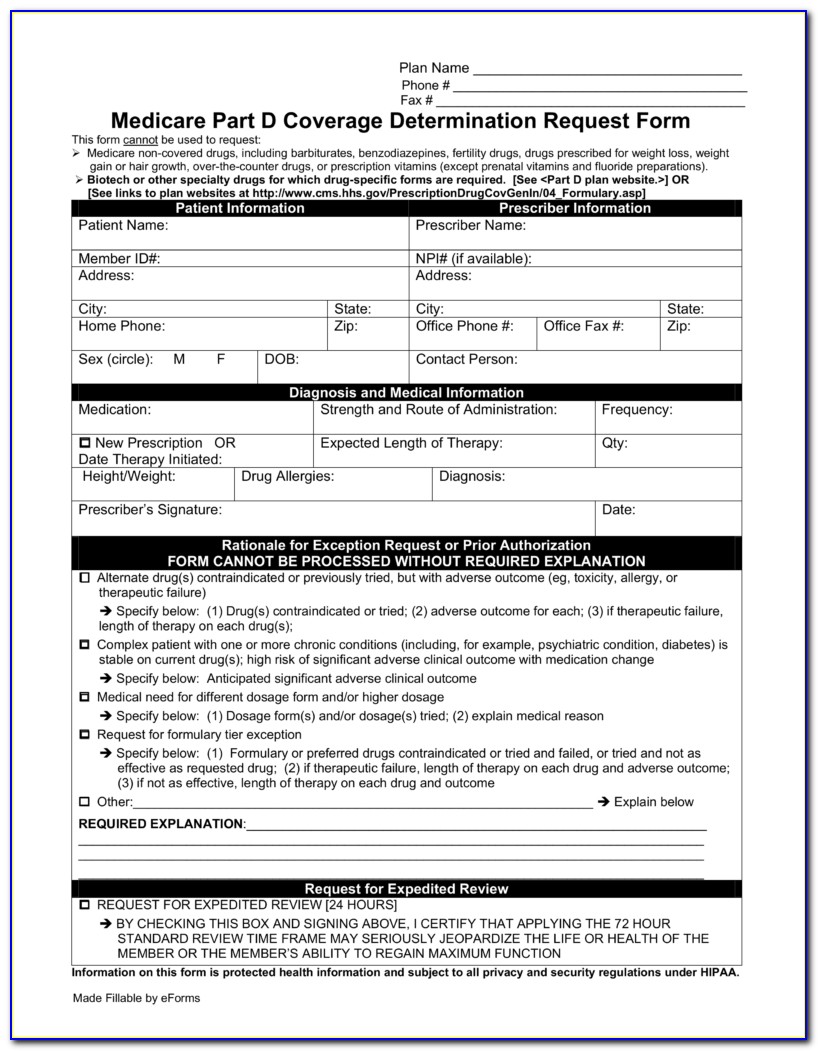
Aetna Medicare Medication Prior Authorization Form Form Resume
Web prior authorization/precertification* request for prescription medications fax this form to: Medical specialty drug prior authorization. You might also hear it called “preapproval” or “precertification”. Please attach supporting information, as necessary, for your request. An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible.
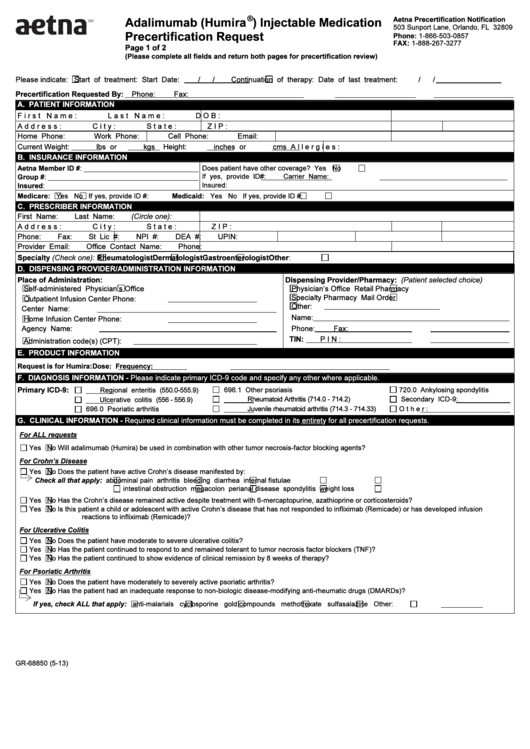
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment: In these cases, your doctor can submit a request on your behalf to get that approval. Web aetna prior (rx) authorization form. Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may.
AZ Care1st Health Plan Treatment Authorization Request 2012 Fill and
Medical specialty drug prior authorization. This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as stated in the. Web aetna prior (rx) authorization form. Web submit your request online at: This is called prior authorization.
Top 6 Aetna Prior Authorization Form Templates free to download in PDF
Within the timeframe outlined in the denial notification. Please attach supporting information, as necessary, for your request. Web aetna prior (rx) authorization form. In these cases, your doctor can submit a request on your behalf to get that approval. This is called prior authorization.
Aetna Prior Authorization Form printable pdf download
In these cases, your doctor can submit a request on your behalf to get that approval. Web aetna prior (rx) authorization form. Please attach supporting information, as necessary, for your request. This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as stated in the..
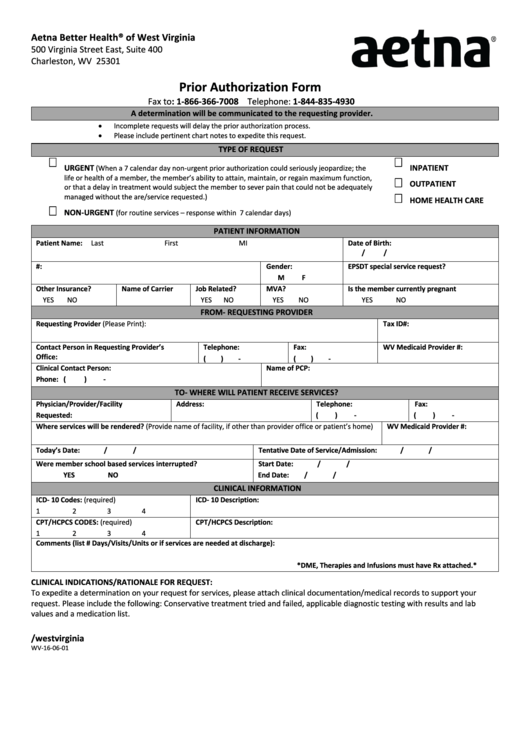
From Wv160601 Aetna Prior Authorization Form printable pdf download
Pharmacy specialty drug prior authorization. This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as stated in the. You might also hear it called “preapproval” or “precertification”. Within the timeframe outlined in the denial notification. Please attach supporting information, as necessary, for your request.
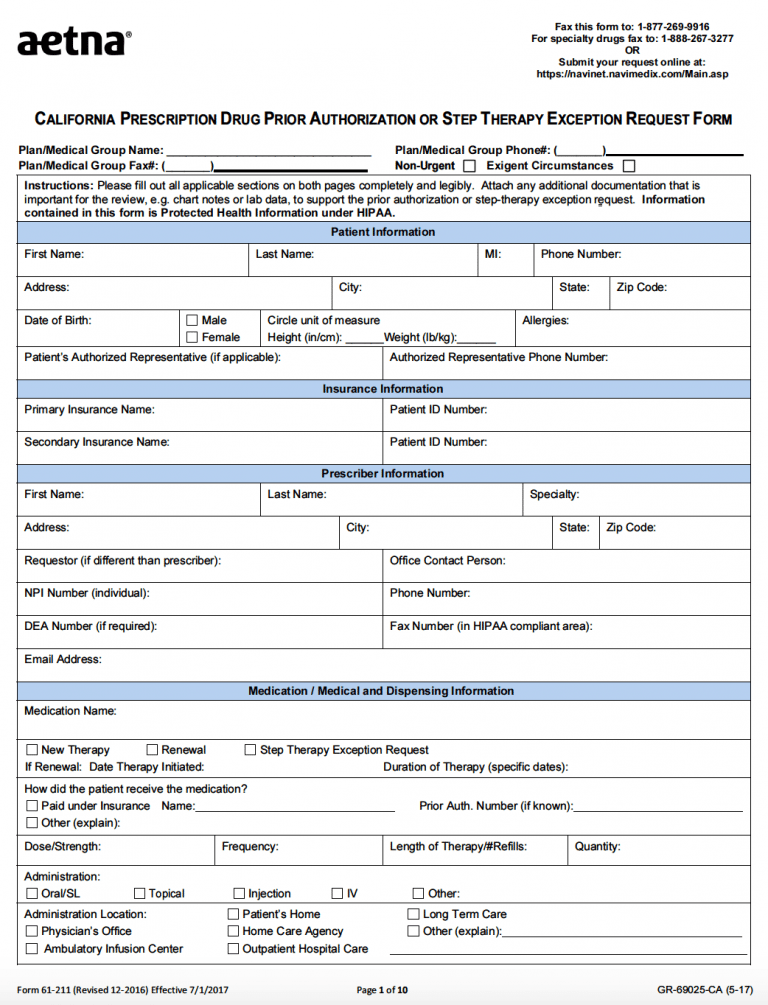
Free AETNA Prior Prescription (Rx) Authorization Form PDF
An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. Please attach supporting information, as necessary, for your request. Pharmacy specialty drug prior authorization. This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as.
Aetna GR690251 CO 20192021 Fill and Sign Printable Template Online
Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Start date / / aetna precertification notification continuation of therapy: Web what is prior authorization? Web aetna prior (rx) authorization form. Medical specialty drug prior authorization.
Aetna Medicare Advantage Disenrollment Form Form Resume Examples
Medical specialty drug prior authorization. Pharmacy specialty drug prior authorization. Within the timeframe outlined in the denial notification. Web prior authorization/precertification* request for prescription medications fax this form to: Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information.
Free Aetna Prior (Rx) Authorization Form PDF eForms
Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment: Web prior authorization/precertification* request for prescription medications fax this form to: This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as stated.
In These Cases, Your Doctor Can Submit A Request On Your Behalf To Get That Approval.
An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. This form asks the medical office for the right to be able to write a prescription to their patient whilst having aetna cover the cost as stated in the. You might also hear it called “preapproval” or “precertification”. This is called prior authorization.
Web Submit Your Request Online At:
Web prior authorization/precertification* request for prescription medications fax this form to: Pharmacy specialty drug prior authorization. Medical specialty drug prior authorization. Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment:
Some Procedures, Tests And Prescriptions Need Prior Approval To Be Sure They’re Right For You.
Web additionally, requests that are subject to prior authorization (or any other utilization management requirement), may require supporting information. Web aetna prior (rx) authorization form. Within the timeframe outlined in the denial notification. Web what is prior authorization?
Start Date / / Aetna Precertification Notification Continuation Of Therapy:
Please attach supporting information, as necessary, for your request.