Bcbs Fep Pharmacy Prior Authorization Form
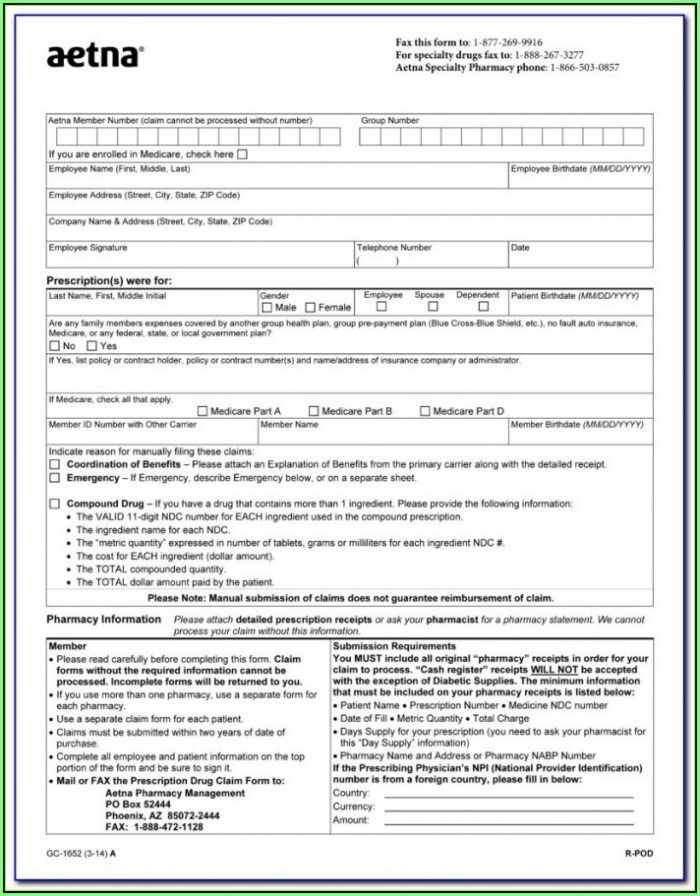
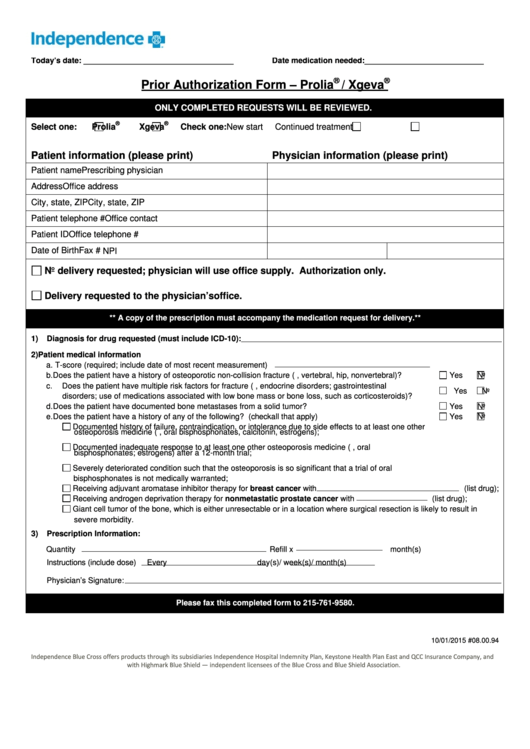
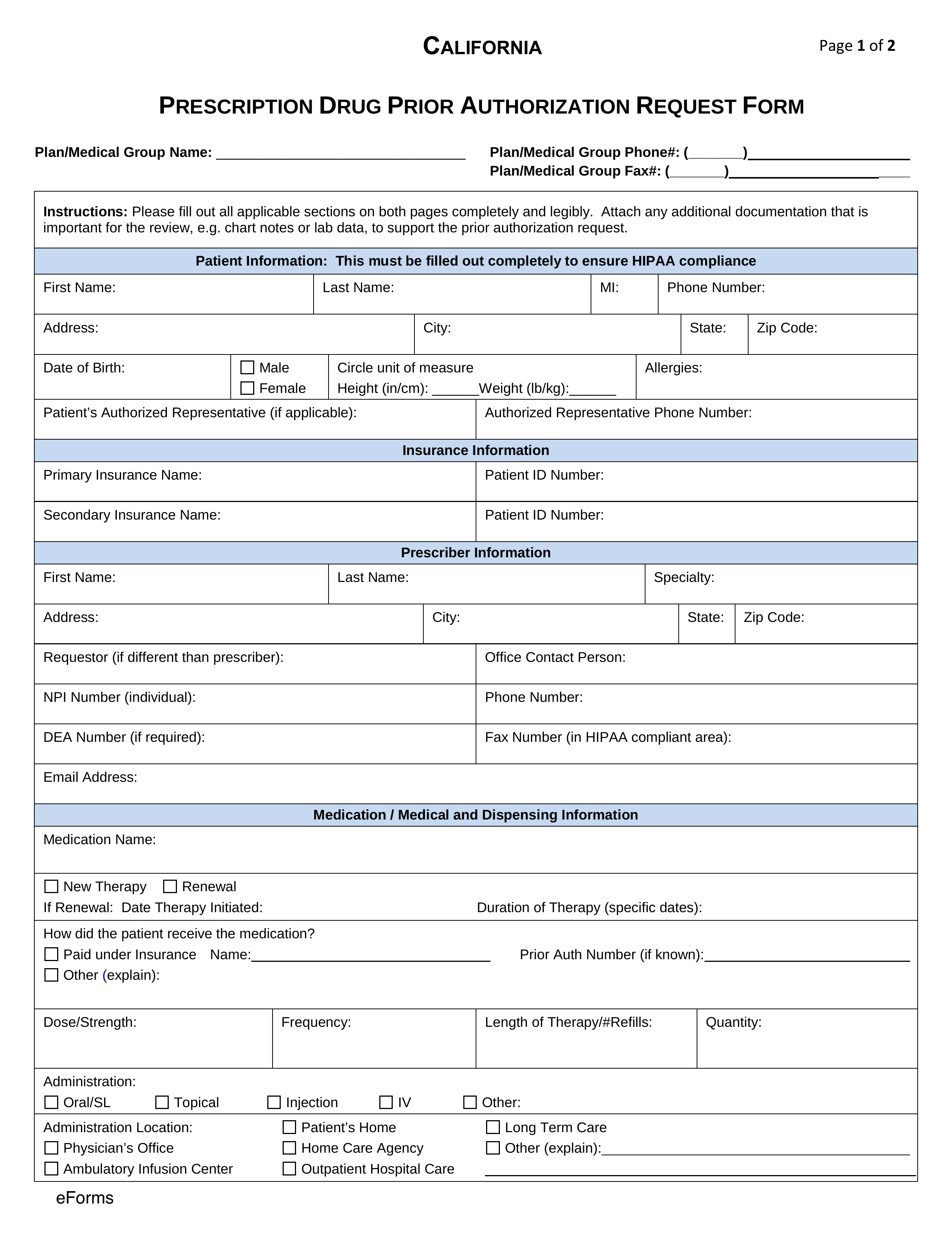
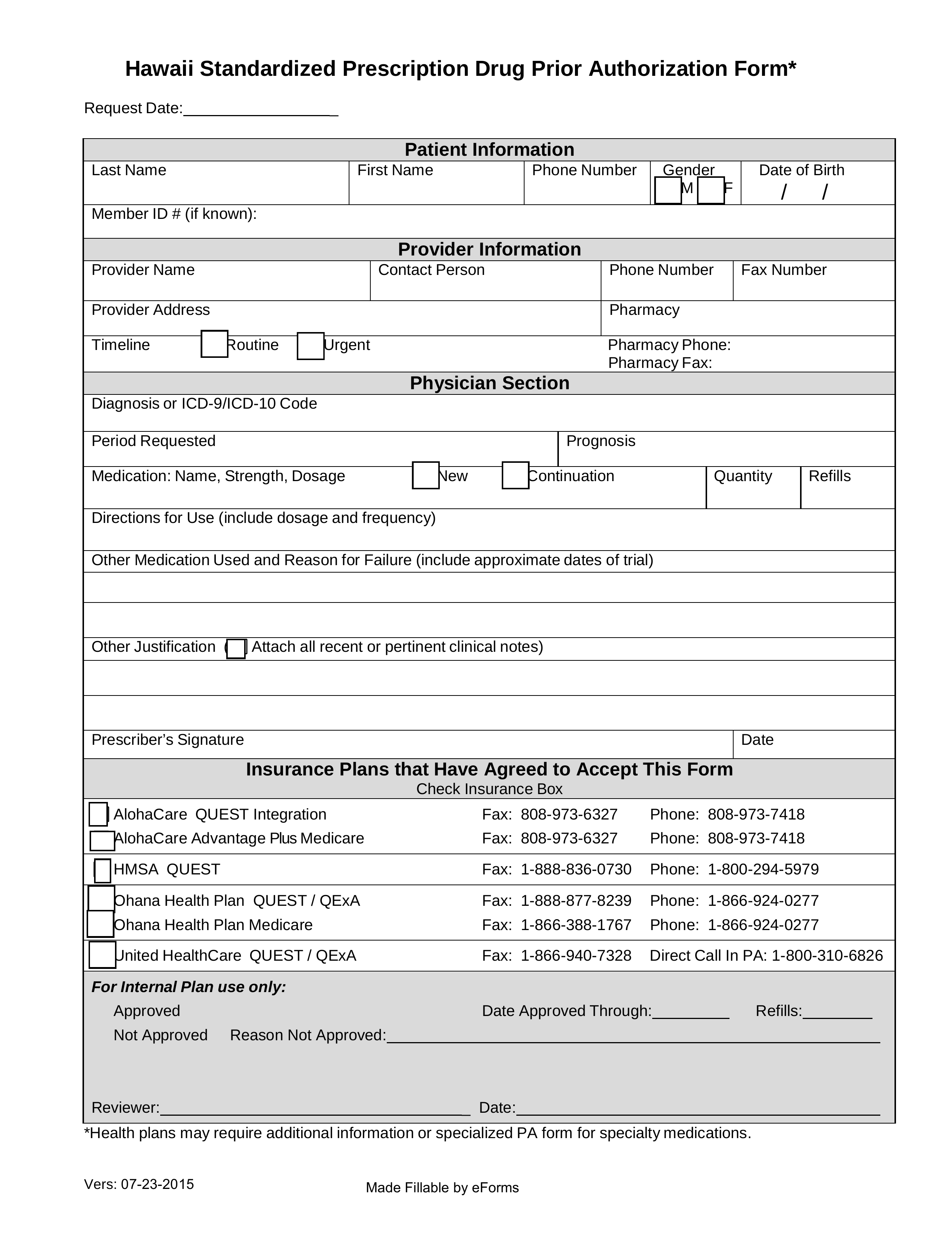
Bcbs Fep Pharmacy Prior Authorization Form - For telephone contacts, please see the blue shield of california member authorizations section on the authorization. Web • pharmacy nabp or npi number or the current name and complete address of pharmacy • full name of the patient • date filled • name of drug, strength (e.g., 500 mg) and. Web director’s office and fep’s own independent pharmacy and therapeutics committee • the pa process is coordinated between cvs caremark and the mail service provider on. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Web or call the number on the back of the member id card. Web premera blue cross is an independent licensee of the blue cross blue shield association serving businesses and residents of alaska and washington state, excluding clark. We’ve recently been inundated with a huge increase in prior authorization (pa) requests. Web for all other questions regarding the submission of your request, please contact cvs caremark: Web your health care provider can request prior approval electronically, by fax or by mail. The increase in requests include an unusual number.
Web premera blue cross is an independent licensee of the blue cross blue shield association serving businesses and residents of alaska and washington state, excluding clark. Web most drugs are covered without requiring prior approval. We’ve recently been inundated with a huge increase in prior authorization (pa) requests. Web federal employee program (fep) medical authorizations. Web blue cross commercial forms. Web or call the number on the back of the member id card. Web select the appropriate fep form to get started. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). To submit a prior authorization.
To submit a prior authorization. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Web federal employee program (fep) medical authorizations. Web select the appropriate fep form to get started. For telephone contacts, please see the blue shield of california member authorizations section on the authorization. Web most drugs are covered without requiring prior approval. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). The full list of drugs that need to be approved, prior approval forms and additional information. Web bcbsaz reserves the right to require prior authorization for such newly released and changed items even though the tool and code lists have not yet been updated to include. Service benefit plan prior approval p.o.
42 Best Bcbs Nc Prior Authorization forms for
Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Web 2023 fep prior approval drug list rev. Get access to over 55,000 retail pharmacies. Web most drugs are covered without requiring prior approval. Web all forms must be signed, then either faxed or mailed.
Bcbs Prior Authorization Form Ohio Form Resume Examples 9lV8N5A30o
Web select the appropriate fep form to get started. However, some select drugs require your doctor to provide information about your prescription to determine. Web to obtain a fax form, visit the prior authorization forms page. Web director’s office and fep’s own independent pharmacy and therapeutics committee • the pa process is coordinated between cvs caremark and the mail service.
Wellpoint Pharmacy Prior Authorization Forms PharmacyWalls
To submit a prior authorization. For telephone contacts, please see the blue shield of california member authorizations section on the authorization. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn. Explore prior approval topics learn about prior. Web all forms must be signed, then either faxed or mailed.
Highmark bcbs member claim form
However, some select drugs require your doctor to provide information about your prescription to determine. Web blue cross and blue shield. Web get the latest from fep. Web all forms must be signed, then either faxed or mailed. Web view and download our medical, pharmacy and overseas claim forms.
Fep Prior Authorization Form â
Your privacy is important to us. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web get the latest from fep. Web the blue cross and blue shield service benefit plan has a variety.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). A prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure,. The full list of drugs that need to be approved, prior approval forms and additional information. Web 2023 fep prior approval drug list rev. Web bcbsaz.
Free California Medicaid Prior (Rx) Authorization Form PDF eForms
Get access to over 55,000 retail pharmacies. Web federal employee program (fep) medical authorizations. Your privacy is important to us. Web view and download our medical, pharmacy and overseas claim forms. Web to obtain a fax form, visit the prior authorization forms page.
Free Hawaii Medicaid Prior (Rx) Authorization Form PDF eForms
The full list of drugs that need to be approved, prior approval forms and additional information. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn. Your privacy is important to us. Be the first to know about our benefits, wellness incentives and rewards you're eligible for with your plan. Explore prior approval topics.
Bcbs Prior Authorization Form Maryland Form Resume Examples Yqlkmob5aj
Blue cross and blue shield of texas (bcbstx) is changing prior authorization requirements for medicare members to reflect new, replaced or removed. We’ve recently been inundated with a huge increase in prior authorization (pa) requests. A prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure,. The full list of drugs that need to.
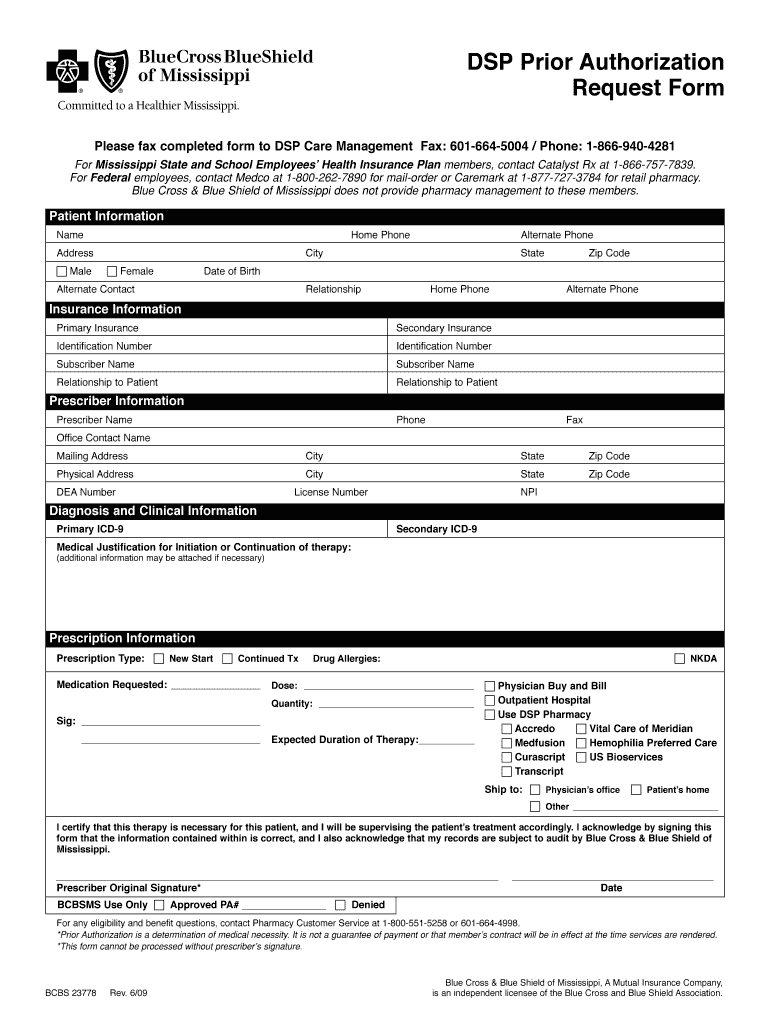
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. To submit a prior authorization. Web most drugs are covered without requiring prior approval. Web the blue cross and blue shield service benefit plan has a variety of.
Web Premera Blue Cross Is An Independent Licensee Of The Blue Cross Blue Shield Association Serving Businesses And Residents Of Alaska And Washington State, Excluding Clark.
Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. To submit a prior authorization. Use the appropriate medication authorization request form below to request prior authorization for a medication that's covered under a member's. Web all forms must be signed, then either faxed or mailed.
Web Or Call The Number On The Back Of The Member Id Card.
The full list of drugs that need to be approved, prior approval forms and additional information. 6 23 23 norditropin noritate northera nourianz novarel noxafil nplate nubeqa nucala nucynta/nucytna er nuedexta numoisyn. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web your health care provider can request prior approval electronically, by fax or by mail.
Web Federal Employee Program (Fep) Medical Authorizations.
Web director’s office and fep’s own independent pharmacy and therapeutics committee • the pa process is coordinated between cvs caremark and the mail service provider on. Web for all other questions regarding the submission of your request, please contact cvs caremark: A prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure,. Web select the appropriate fep form to get started.
Web Bcbsaz Reserves The Right To Require Prior Authorization For Such Newly Released And Changed Items Even Though The Tool And Code Lists Have Not Yet Been Updated To Include.
Explore prior approval topics learn about prior. Your privacy is important to us. Web get the latest from fep. Web blue cross and blue shield.