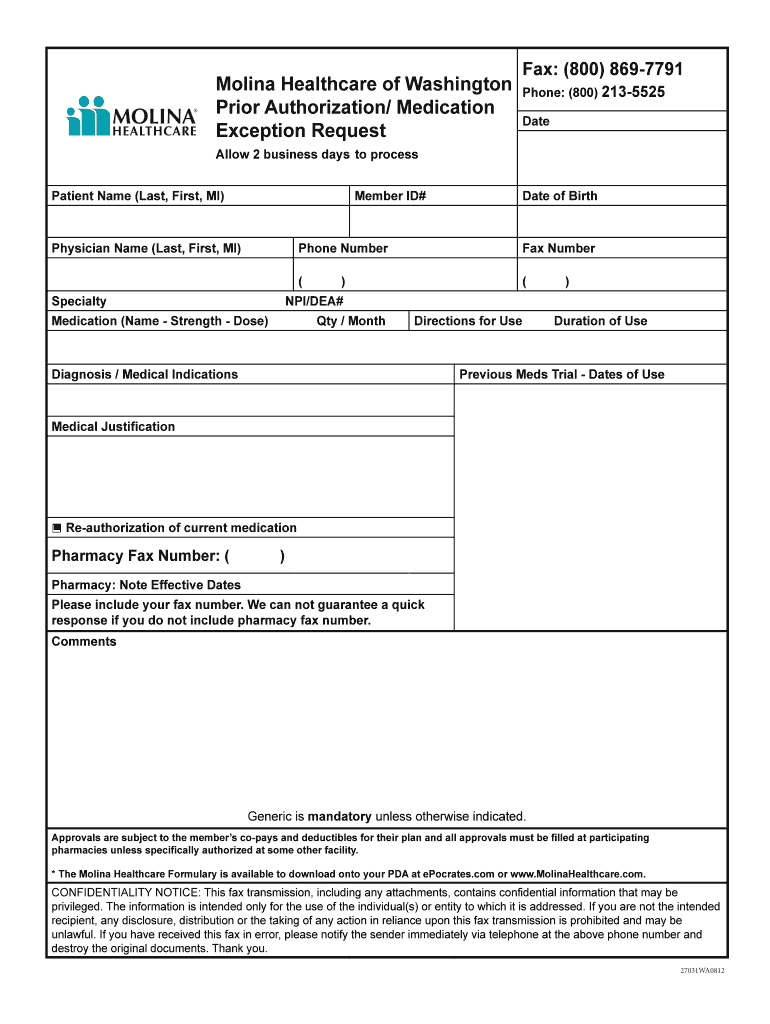
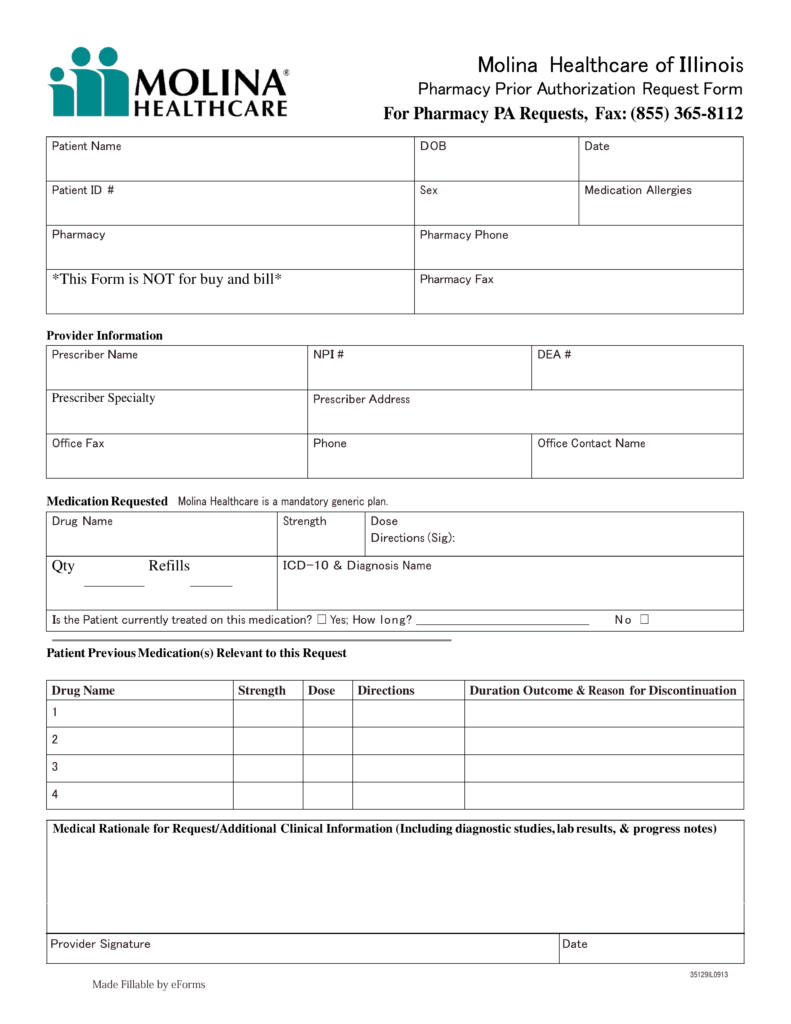
Molina Medication Prior Authorization Form
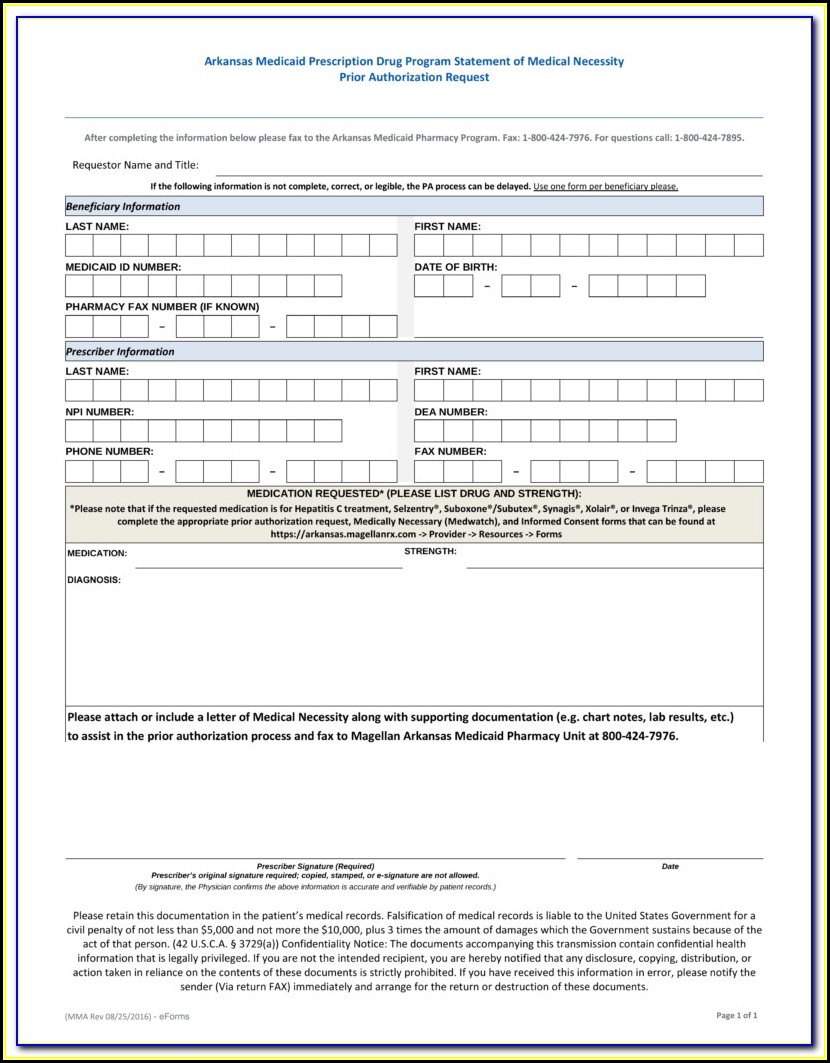
Molina Medication Prior Authorization Form - Edit, sign and save prior authorization req form. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. ☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web prior authorization lookup tool. Pharmacy prior authorization forms ; Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests, fax: Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Web drug prior authorization form michigan medicaid and marketplace phone:
Molina healthcare prior authorization request form and instructions. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. ☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. Web the preferred drug list and the pdl criteria guide can be found here. Progress notes cholesterol lowering (ie. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Edit, sign and save prior authorization req form. Pharmacy prior authorization forms ; It is needed before you can get certain services or drugs. It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed.
It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. Pharmacy prior authorization forms ; The forms are also available on the frequently used forms page. It is needed before you can get certain services or drugs. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Please enter one email address * email this article to: Please see the clinical pa criteria that molina has implemented below. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Items on this list will only be dispensed after prior authorization from molina healthcare. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit.
Molina Authorization Form Fill Online, Printable, Fillable, Blank
Edit, sign and save prior authorization req form. Progress notes cholesterol lowering (ie. Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Pdffiller allows users to edit, sign, fill & share all type of.
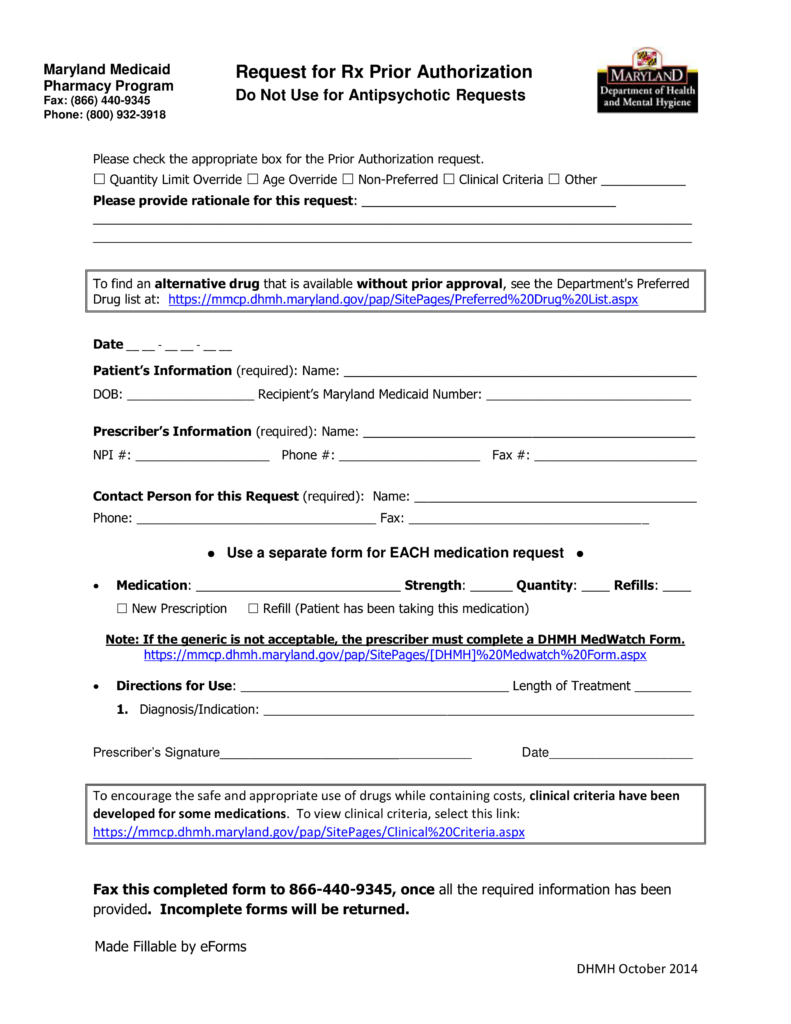
Free Maryland Medicaid Prior (Rx) Authorization Form PDF eForms
Please enter one email address * email this article to: Web drug prior authorization form michigan medicaid and marketplace phone: The forms are also available on the frequently used forms page. It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. Pharmacy prior authorization forms ;
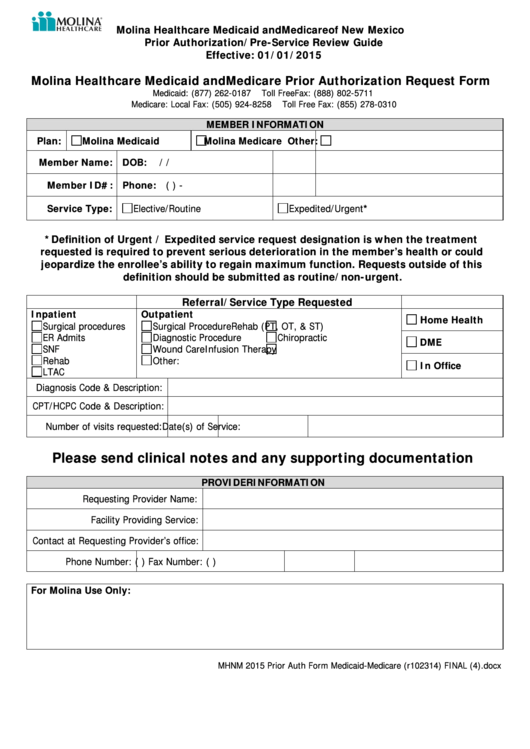
UT Molina Healthcare Prior Authorization Form 20162022 Fill and Sign
☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. It is needed before you can get certain services or drugs. Please enter one email address * email this article to: Web drug prior authorization form michigan medicaid and marketplace phone: Pdffiller allows users to edit, sign, fill & share all type of documents online.
Molina Healthcare Medicaid And Medicare Prior Authorization Request
The forms are also available on the frequently used forms page. It is needed before you can get certain services or drugs. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Web the preferred drug list and the pdl criteria guide can be found here. Please enter one email address.
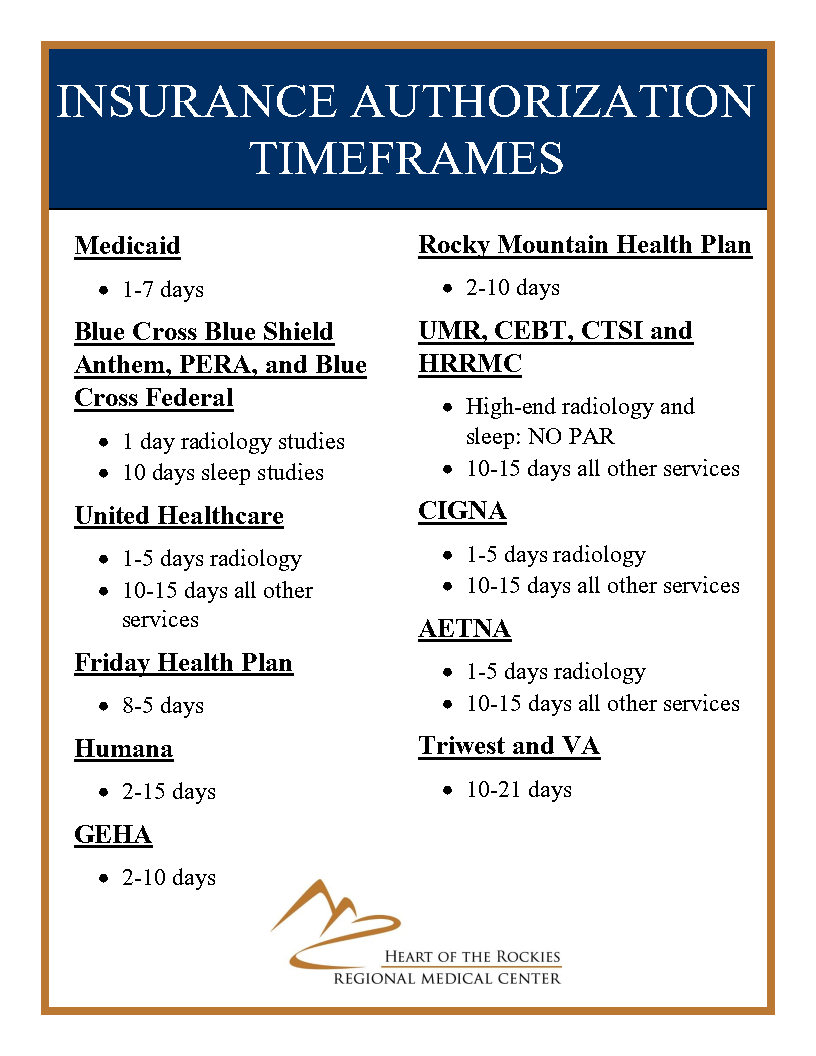
Insurance Prior Authorization Timeframes Medical Center in Salida
Pharmacy prior authorization forms ; Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are.
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit. Please see the clinical pa criteria that molina has implemented below. Pharmacy prior authorization forms ; Molina healthcare prior authorization request form and instructions. Please enter one email address * email this article to:
Molina Medicare Medication Prior Authorization Form Form Resume
Web the preferred drug list and the pdl criteria guide can be found here. Molina healthcare prior authorization request form and instructions. The forms are also available on the frequently used forms page. Pharmacy prior authorization forms ; Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests, fax:
Molina Healthcare Medication Prior Authorization/Exceptions Request
It is needed before you can get certain services or drugs. Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Molina healthcare prior authorization request form and instructions. Please enter one email address * email this article to: Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of.
Molina Medicare Medication Prior Authorization Form Form Resume
Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Pharmacy prior authorization forms ; Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web molina healthcare of illinois pharmacy prior.
Prior Authorization Form For Molina Medicare Universal Network
Web prior authorization lookup tool. It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web drug prior authorization form michigan medicaid and marketplace phone: Please see the clinical pa.
Edit, Sign And Save Prior Authorization Req Form.
☐ new request ☐ reauthorization patient previous medication(s) relevant to this request (complete for. 01/01/2022 for dual members with medicaid, please refer to your state medicaid pa guide for additional pa requirements refer to molina’s provider website or prior. Web the preferred drug list and the pdl criteria guide can be found here. Web molina healthcare of illinois pharmacy prior authorization request form for pharmacy pa requests, fax:
Pharmacy Prior Authorization Forms ;
Please enter one email address * email this article to: Items on this list will only be dispensed after prior authorization from molina healthcare. It is needed before you can get certain services or drugs. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription.
Progress Notes Cholesterol Lowering (Ie.
Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Pdffiller allows users to edit, sign, fill & share all type of documents online. It should be noted that the medical office will need to provide justification for requesting the specific medication, and that authorization is not guaranteed. Web prior authorization lookup tool.
Web Members > Medicaid > About Medicaid > Getting Care > Prior Authorizations Prior Authorizations What Are Prior Authorizations?
Formulary drugs (formulary drug search here ) may require a clinical prior authorization. Molina healthcare prior authorization request form and instructions. The forms are also available on the frequently used forms page. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’ pharmacy benefit.