Triwest Appeal Form
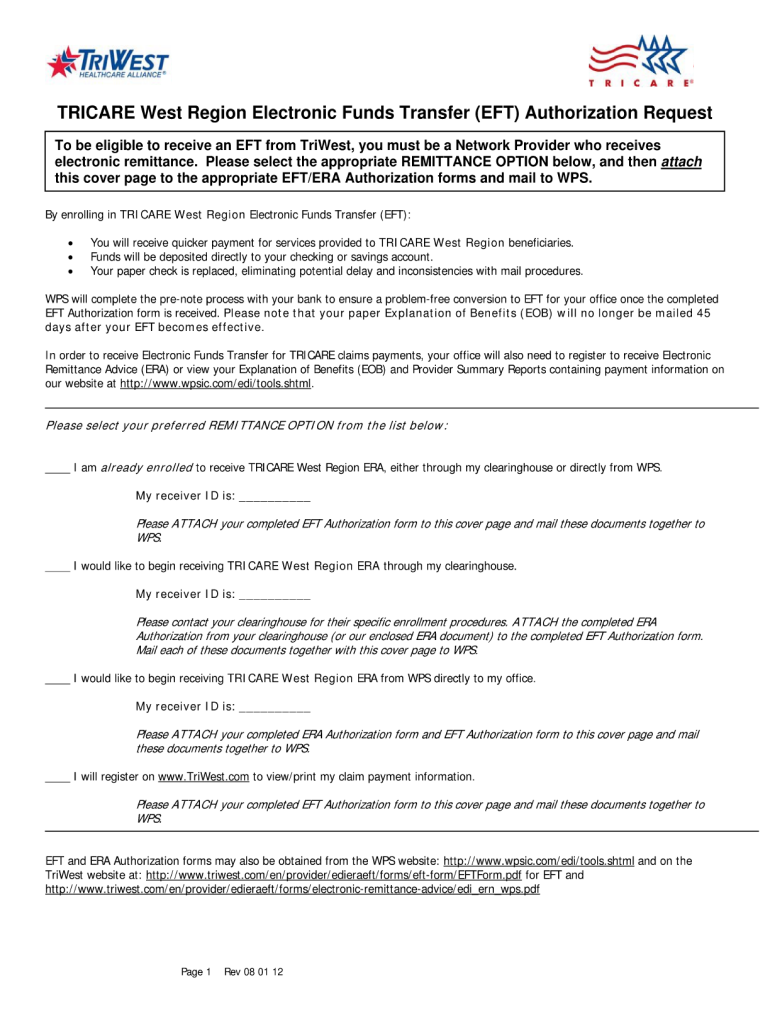
Triwest Appeal Form - You will be able to print the form and obtain a tracking number after submission. Click on the resources tab, select the pgba edi provider trading partner agreement, complete the forms and follow the instructions to submit them by either fax or mail. Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans affairs (va) in administering the community care programs. Incomplete or missing information on forms could result in a denial for not meeting va’s timely filing requirements. Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary You will be able to print a preview of your appeal before it is submitted and a copy of the submitted appeal with a tracking number. Enroll for eft/era proudly caring for our nation's heroes Web you may use the online appeal submission form below or submit an appeal letter via mail or fax. Ccn pc3 reason for provider reconsideration request (select one): Web home » provider services community care network providers enroll online for eft/era for faster payments say goodbye to waiting for mailed checks to arrive with online eft/era enrollment in a new fast, secure app on the availity essentials page.
Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans affairs (va) in administering the community care programs. Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary Previous section print this preview submitter information relationship to patient / beneficiary relationship description: Incomplete or missing information on forms could result in a denial for not meeting va’s timely filing requirements. Claim originally sent to the following (check one): Va optum triwest date of previous claim submission: Web you may use the online appeal submission form below or submit an appeal letter via mail or fax. You will be able to print a preview of your appeal before it is submitted and a copy of the submitted appeal with a tracking number. Web claim forms claim rejection letter mail the completed form and all supporting documentation to: Providers can submit electronic claims without a clearinghouse account.
Web claim forms claim rejection letter mail the completed form and all supporting documentation to: Ccn pc3 reason for provider reconsideration request (select one): Claim originally sent to the following (check one): Web to enroll in edi claims submission, log in to the triwest payer space on availity.com. Providers can submit electronic claims without a clearinghouse account. Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary Click on the resources tab, select the pgba edi provider trading partner agreement, complete the forms and follow the instructions to submit them by either fax or mail. Web to submit an appeal, download triwest's provider claims reconsideration form, available under the resources tab on the triwest payer space on availity. Web home » provider services community care network providers enroll online for eft/era for faster payments say goodbye to waiting for mailed checks to arrive with online eft/era enrollment in a new fast, secure app on the availity essentials page. You will be able to print the form and obtain a tracking number after submission.
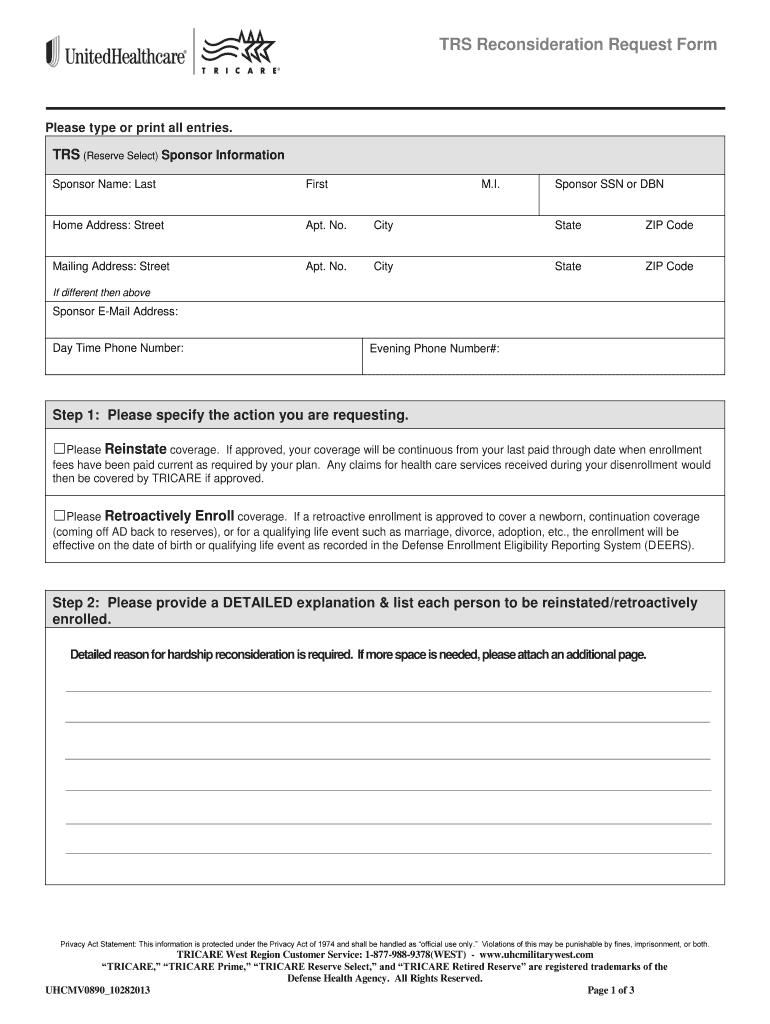
Triwest Reconsideration Form Fill Online, Printable, Fillable, Blank
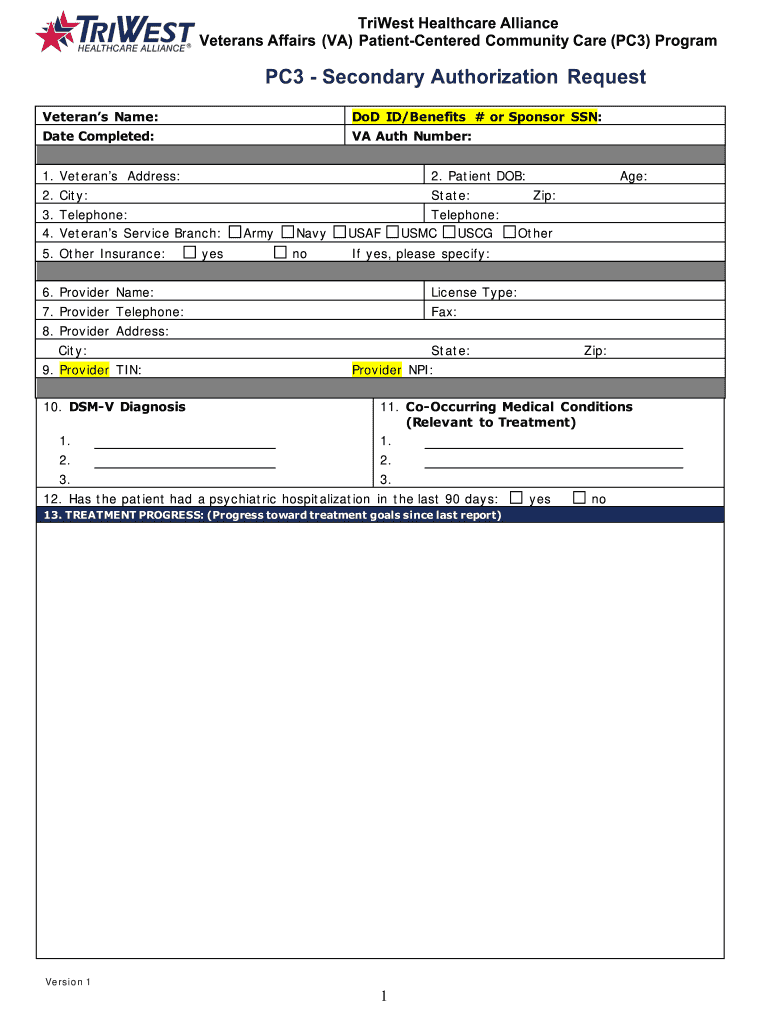
Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans affairs (va) in administering the community care programs. Previous section print this preview submitter information relationship to patient / beneficiary relationship description: Web to submit an appeal, download triwest's provider claims reconsideration form, available under the resources tab on.
Rehab Insurance Triwest insurance coverage for Veterans
Web claim forms claim rejection letter mail the completed form and all supporting documentation to: Claim originally sent to the following (check one): Click on the resources tab, select the pgba edi provider trading partner agreement, complete the forms and follow the instructions to submit them by either fax or mail. You will be able to print the form and.
Tricare Appeal Form Pdf Fill Online, Printable, Fillable, Blank
Providers can submit electronic claims without a clearinghouse account. To submit a claim reconsideration, you must submit separate appeals for each disputed item. Web you may use the online appeal submission form below or submit an appeal letter via mail or fax. Web claim forms claim rejection letter mail the completed form and all supporting documentation to: Claim originally sent.
TriWest Capital Olson Silver Company
Click on the resources tab, select the pgba edi provider trading partner agreement, complete the forms and follow the instructions to submit them by either fax or mail. You will be able to print a preview of your appeal before it is submitted and a copy of the submitted appeal with a tracking number. You will be able to print.
TriWest SAR15 Fill and Sign Printable Template Online US Legal Forms
Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary Web home » provider services community care network providers enroll online for eft/era for faster payments say goodbye to waiting for mailed checks to arrive with online eft/era enrollment in a new fast, secure app on the availity essentials page. Claim originally sent.
AZ Big Media TriWest Corporate Headquarters Campus sold to private
You will be able to print the form and obtain a tracking number after submission. Ccn pc3 reason for provider reconsideration request (select one): Web to submit an appeal, download triwest's provider claims reconsideration form, available under the resources tab on the triwest payer space on availity. You will be able to print a preview of your appeal before it.
TriWest Healthcare Alliance will add 500 jobs in Kansas City by Sept. 8
Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary Enroll for eft/era proudly caring for our nation's heroes Claim originally sent to the following (check one): Providers can submit electronic claims without a clearinghouse account. Web claim forms claim rejection letter mail the completed form and all supporting documentation to:
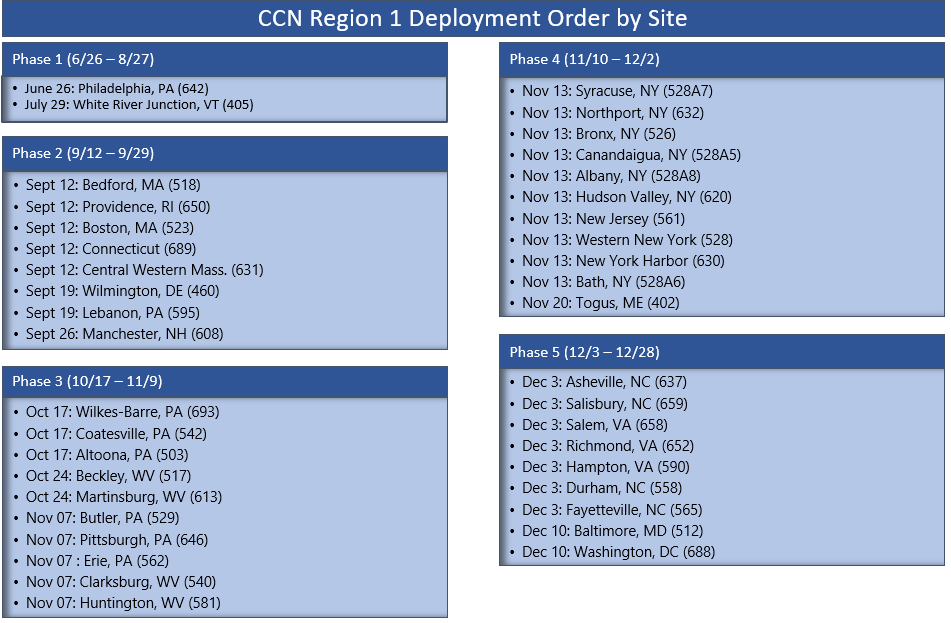
Issue 10 VHA Office of Community Care Monthly Provider Updates
Ccn pc3 reason for provider reconsideration request (select one): Web you may use the online appeal submission form below or submit an appeal letter via mail or fax. Claim originally sent to the following (check one): Web welcome from triwest healthcare alliance. Click on the resources tab, select the pgba edi provider trading partner agreement, complete the forms and follow.
Triwest Authorization Request Form Fill Out and Sign Printable PDF
Web you may use the online appeal submission form below or submit an appeal letter via mail or fax. Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary Web to enroll in edi claims submission, log in to the triwest payer space on availity.com. Previous section print this preview submitter information relationship.
TriWest Choice Contracting
To submit a claim reconsideration, you must submit separate appeals for each disputed item. Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans affairs (va) in administering the community care programs. Va optum triwest date of previous claim submission: Web to submit an appeal, download triwest's provider claims.
Ccn Pc3 Reason For Provider Reconsideration Request (Select One):
Web to submit an appeal, download triwest's provider claims reconsideration form, available under the resources tab on the triwest payer space on availity. Va optum triwest date of previous claim submission: Web you may use the online appeal submission form below or submit an appeal letter via mail or fax. You will be able to print the form and obtain a tracking number after submission.
Web Welcome From Triwest Healthcare Alliance.
Complete our online appeal form. Web home » provider services community care network providers enroll online for eft/era for faster payments say goodbye to waiting for mailed checks to arrive with online eft/era enrollment in a new fast, secure app on the availity essentials page. Web to enroll in edi claims submission, log in to the triwest payer space on availity.com. To submit a claim reconsideration, you must submit separate appeals for each disputed item.
Claim Originally Sent To The Following (Check One):
Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans affairs (va) in administering the community care programs. You will be able to print a preview of your appeal before it is submitted and a copy of the submitted appeal with a tracking number. Enroll for eft/era proudly caring for our nation's heroes Click on the resources tab, select the pgba edi provider trading partner agreement, complete the forms and follow the instructions to submit them by either fax or mail.
Incomplete Or Missing Information On Forms Could Result In A Denial For Not Meeting Va’s Timely Filing Requirements.
Web claim forms claim rejection letter mail the completed form and all supporting documentation to: Previous section print this preview submitter information relationship to patient / beneficiary relationship description: Providers can submit electronic claims without a clearinghouse account. Authorization or claim denied as not a covered benefit authorization or claim denied as not medically necessary